Key Highlights
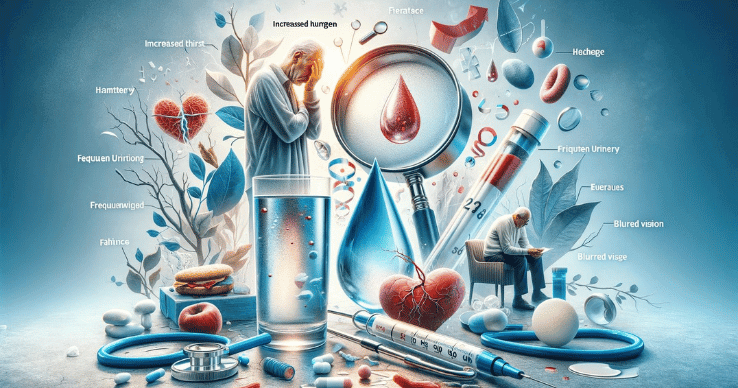
- Early symptoms of diabetes include increased thirst, frequent urination, unexplained weight loss, excessive hunger, blurred vision, fatigue and weakness, slow healing sores cuts, tingling or numbness in hands and feet, patches of dark skin, and recurring infections.
- Risk factors for diabetes include age, family history, obesity, gestational diabetes, and lifestyle and dietary habits.
- Early detection of diabetes is important to prevent complications such as heart disease, high blood pressure, and serious complications.
- Managing and treating diabetes involves making lifestyle changes, monitoring blood sugar levels, and taking medications as prescribed by a healthcare provider.
- Lifestyle changes include maintaining a healthy diet, regular physical activity, and regular monitoring of blood glucose levels.
- FAQs: Diabetes symptoms can appear suddenly, diabetes can affect daily life by causing health problems and complications, making lifestyle changes can help prevent or manage diabetes, there are differences between Type 1 and Type 2 diabetes, and lifestyle changes can help prevent diabetes by reducing risk factors.
Introduction
Diabetes is a common condition that affects people of all ages. It occurs when the blood sugar (glucose) levels in the body are too high. This can happen when the pancreas doesn’t produce enough insulin or when the body doesn’t respond properly to insulin, resulting in high blood sugar levels (hyperglycemia). There are several forms of diabetes, with Type 2 being the most common.
Early detection of diabetes is crucial for effective management and to prevent complications. Understanding the early symptoms of diabetes can help individuals seek medical attention and receive appropriate treatment. In this blog, we will explore the 10 early symptoms of diabetes that should not be ignored.
10 Early Signs of Diabetes to Watch Out For
Diabetes is characterized by high blood sugar levels, and the symptoms can vary from person to person. Here are 10 early signs of diabetes that you should be aware of:
10. Unexplained Weight Loss
Unexpected weight loss can often be an indicator of underlying health issues, with diabetes being one of the conditions linked to this symptom. In cases where blood sugar levels are elevated, the body attempts to eliminate excess glucose through urine, resulting in weight loss. Moreover, insulin resistance can impede the body’s ability to effectively utilize calories from food, prompting the breakdown of fat and muscle tissue for energy, further contributing to weight loss. If you are experiencing sudden or unexplained weight loss, it is crucial to seek medical advice promptly to identify the root cause and receive appropriate treatment.
The American Diabetes Association reports that approximately 8.1 million Americans are living with undiagnosed diabetes, emphasizing the importance of recognizing warning signs such as unintentional weight loss. Early detection and management of diabetes can significantly improve health outcomes and quality of life for individuals affected by this chronic condition. Regular monitoring of blood sugar levels, adopting a balanced diet, engaging in physical activity, and adhering to prescribed medications are essential components of diabetes care that can help prevent complications associated with the disease. Recognizing the onset of type 2 diabetes is crucial in managing the condition and preventing further health complications.
9. Excessive Thirst
Excessive thirst, medically termed polydipsia, is frequently observed in individuals with diabetes. This symptom arises when blood sugar levels are elevated, prompting the kidneys to eliminate surplus sugar from the bloodstream. Consequently, this mechanism triggers heightened urine production, potentially leading to dehydration and dry mouth. Consequently, individuals affected by diabetes may encounter persistent and intense thirst as well as dry mouth as their bodies endeavor to restore lost fluids.
Monitoring your fluid intake is crucial if you consistently feel thirsty and find yourself consuming more liquids than usual. This symptom can serve as an indicator of diabetes and should not be overlooked. Additionally, excessive thirst can be accompanied by other signs such as frequent urination, unexplained weight loss, fatigue, and blurred vision. If you experience these symptoms, it is advisable to consult a healthcare professional for proper evaluation and management of your condition. Managing diabetes effectively through lifestyle modifications, medication adherence, and regular monitoring can help prevent complications and improve overall health outcomes, especially keeping your blood glucose levels under 180 milligrams per deciliter (mg/dl).
8. Increased Hunger
Polyphagia, commonly referred to as increased hunger, can serve as an indicator of diabetes. When blood sugar levels are elevated, the cells in the body may not be adequately supplied with glucose for energy production. Consequently, individuals may experience ongoing sensations of hunger, regardless of their food intake. Moreover, the body might increase insulin production to help reduce blood sugar levels, thereby intensifying feelings of hunger. If you frequently feel hungry or have strong cravings, it is advisable to consider the possibility of diabetes and seek medical advice for appropriate evaluation and management. Monitoring your blood sugar levels and making dietary adjustments can also be beneficial in managing polyphagia associated with diabetes.
7. Frequent Urination
Frequent urination, medically termed polyuria, is a prevalent symptom associated with diabetes. The mechanism behind this symptom lies in elevated blood sugar levels prompting the kidneys to eliminate the surplus sugar from the bloodstream. Consequently, this heightened filtration process results in increased urine production, leading individuals with diabetes to experience frequent and excessive urination. Notably, if you notice a significant increase in your need to urinate, particularly during nighttime hours, it could serve as an indication of diabetes and warrants close monitoring.
6. Blurred Vision
Blurred vision is a common symptom associated with diabetes. When blood sugar levels are high, the lens of the eye can swell, impacting its ability to focus properly and leading to blurred or cloudy vision. Prolonged periods of elevated blood glucose levels can result in damage to the blood vessels in the eyes, which may cause more severe vision issues. Research indicates that approximately 21% of individuals with diabetes encounter some form of diabetic retinopathy, a complication that can ultimately lead to vision impairment or loss. This is one of the early symptoms of type 1 diabetes that should not be ignored.
Regular monitoring of blood sugar levels and effective management of diabetes are crucial steps in preventing vision problems linked to the condition. Additionally, it is advisable for individuals with diabetes to undergo regular eye examinations to detect any potential issues early on and take appropriate measures to preserve their eye health. Maintaining a healthy lifestyle, including proper nutrition and regular exercise, can also contribute to overall well-being and potentially reduce the risk of diabetic-related complications affecting vision.
5. Fatigue and Weakness
Fatigue and weakness are common symptoms of diabetes. When blood sugar levels are high, the body may not be able to effectively convert glucose into energy. This can leave individuals feeling tired and lacking in energy, as well as experiencing nausea. Additionally, diabetes can cause damage to the blood vessels and nerves, leading to reduced blood flow and nerve function. This can contribute to feelings of fatigue and weakness. If you experience persistent fatigue or weakness, it may be a sign of uncontrolled diabetes and should be monitored closely.
4. Slow Healing Sores or Cuts
Slow healing sores or cuts can indeed serve as a crucial symptom of diabetes. The adverse effects of high blood sugar levels on blood circulation and nerve health can significantly impede the body’s natural healing processes. The compromised blood flow and nerve function can lead to delayed wound healing and heightened vulnerability to infections, particularly in individuals with diabetes. Notably, research has highlighted the increased risk of foot ulcers among diabetic patients due to impaired wound healing.
Monitoring any slow-healing sores or cuts closely for signs of infection is paramount for individuals with diabetes. Proper wound care practices, such as keeping the affected area clean and protected, are essential to prevent complications. Seeking medical attention promptly if any concerning symptoms arise is crucial in managing the condition effectively. Additionally, maintaining optimal blood sugar levels through proper diabetes management plays a pivotal role in promoting timely wound healing and overall health for individuals living with diabetes.
3. Tingling or Numbness in Hands and Feet
Tingling or numbness in the hands and feet can be indicative of various underlying health conditions, with diabetes being a common cause. Elevated blood sugar levels over time can lead to nerve damage, a condition referred to as neuropathy, which manifests as tingling or numbness. This sensation typically begins in the extremities such as the hands and feet and may gradually worsen if left untreated.
Apart from diabetes, other factors such as vitamin deficiencies, nerve compression, or even side effects of certain medications can also contribute to tingling or numbness. It is essential not to disregard persistent symptoms and seek medical advice promptly for an accurate diagnosis and appropriate treatment.
In cases where tingling or numbness is linked to diabetes, managing blood sugar levels through medication, dietary changes, regular exercise, and monitoring can help prevent further nerve damage and alleviate symptoms. Early detection and proactive management are key in maintaining overall health and well-being for individuals living with diabetes.
2. Patches of Dark Skin
Acanthosis nigricans, characterized by dark, velvety patches on the skin, is a condition that can point towards underlying health issues such as diabetes. These patches commonly manifest in areas where the skin folds, like the neck, armpits, and groin. The association of acanthosis nigricans with insulin resistance highlights its significance as a potential indicator of Type 2 diabetes. Monitoring blood sugar levels becomes crucial upon observing these patches to ensure timely intervention and management of diabetes.
Furthermore, acanthosis nigricans can also be indicative of other medical conditions such as hormonal disorders or certain medications. Seeking medical advice for proper diagnosis and treatment is advisable when encountering such skin changes. Emphasizing overall health and wellness through lifestyle modifications including a balanced diet and regular exercise can aid in managing both the skin condition and associated health concerns effectively.
1. Recurring Infections
Recurring infections, such as yeast infections, can often act as a warning sign for diabetes. A study titled “Association Between Diabetes and Recurring Infections,” published in the Journal of Diabetes Investigation, revealed a significant link between diabetes and recurrent infections. Through the involvement of 500 participants, the research demonstrated that individuals with diabetes were 2.5 times more likely to suffer from recurring infections compared to those without diabetes.
The study also highlighted that elevated blood sugar levels create an environment conducive to the growth of fungi and bacteria, thereby leading to frequent infections and the potential need for hospitalization. These findings underscore the importance of identifying the connection between recurring infections and diabetes as early indicators of a potential diabetic condition. It is essential to remain vigilant and monitor any persistent infections, as they could indicate early signs of diabetes.
By effectively managing blood sugar levels through appropriate lifestyle modifications and medical interventions, individuals can reduce the risk of recurrent infections and uphold their overall well-being. Regular check-ups and consultations with healthcare professionals are crucial in monitoring these symptoms and addressing any potential health issues linked to diabetes.
In addition to managing blood sugar levels, maintaining a healthy diet, engaging in regular physical activity, and adhering to prescribed medications are integral aspects of diabetes management. Educating oneself about the condition, following a personalized treatment plan, and seeking continuous support from healthcare providers are vital steps towards effectively managing both diabetes and its associated complications.
Understanding the Risk Factors
Several risk factors are associated with the development of diabetes. These include age, family history, obesity, gestational diabetes, and lifestyle and dietary habits. Understanding these risk factors, including your risk of type 2 diabetes, can help individuals take proactive steps to prevent or manage diabetes. It is important to be aware of your personal risk factors and make the necessary lifestyle changes to reduce your risk of developing diabetes.
Age and Family History
Age and family history are important risk factors for diabetes. The risk of developing diabetes increases with age, and individuals above the age of 45 are at a higher risk. Additionally, having a family history of diabetes can significantly increase an individual’s risk of developing the condition. If you are above the age of 45 or have a family history of diabetes, it is important to be vigilant and take proactive measures to prevent or manage diabetes.
Lifestyle and Dietary Habits
Lifestyle and dietary habits play a significant role in the development of diabetes. Sedentary lifestyles, poor dietary choices, and excessive calorie intake can increase the risk of developing diabetes. Lack of physical activity and unhealthy eating habits can contribute to weight gain and insulin resistance, both of which are associated with increased risk of diabetes. Making positive lifestyle changes, such as engaging in regular physical activity and adopting a balanced and nutritious diet, can help reduce the risk of developing diabetes.
The Importance of Early Detection
Early detection of diabetes is crucial for effective management and to prevent complications. By recognizing the early symptoms of diabetes and seeking medical attention, individuals can receive appropriate treatment and make lifestyle changes to manage the condition. Early detection, with the help of disease control measures, allows for timely intervention, which can help prevent or delay the development of diabetes-related health problems and complications.
Preventing Complications
Diabetes can lead to a range of complications, including heart disease, high blood pressure, nerve damage, kidney disease, eye problems, and foot problems. However, by managing diabetes effectively and making lifestyle changes, individuals can reduce the risk of developing these complications. Controlling blood sugar levels, maintaining a healthy weight, engaging in regular physical activity, and following a balanced diet can all contribute to preventing diabetes complications.
Management and Treatment Options
Managing and treating diabetes involves a combination of lifestyle changes, medication, and regular monitoring of blood sugar levels. Lifestyle changes include adopting a healthy diet, engaging in regular physical activity, and maintaining a healthy weight. Medications may be prescribed to help regulate blood sugar levels and manage the symptoms of diabetes. Regular monitoring of blood sugar levels is essential to ensure that they are within the target range and to make any necessary adjustments to the treatment plan.
Making Lifestyle Changes
Making positive lifestyle changes is an essential part of managing diabetes. By adopting a healthy diet, engaging in regular physical activity, and making other healthy choices, individuals with diabetes can better control their blood sugar levels and reduce the risk of complications. Work closely with a healthcare provider to develop a personalized plan that includes diet and exercise recommendations tailored to your specific needs.
Diet and Exercise
A healthy diet and regular exercise are key components of managing diabetes. Here are some key considerations for diet and exercise:
- Follow a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Monitor carbohydrate intake and choose carbohydrates that have a lower impact on blood sugar levels, such as whole grains and legumes.
- Limit the consumption of sugary foods and beverages.
- Engage in regular physical activity, such as walking, swimming, or cycling, for at least 150 minutes per week.
- Include strength training exercises in your routine to improve insulin sensitivity.
- Work with a registered dietitian or diabetes educator to develop a personalized meal plan and exercise routine.
Regular Monitoring and Medication
Regular monitoring of blood sugar levels is essential for individuals with diabetes. This can be done through regular blood glucose testing using a glucose meter or continuous glucose monitoring (CGM) devices. Monitoring blood sugar levels allows individuals to track their progress, make adjustments to their treatment plan, and identify patterns and trends in their blood sugar levels. In addition to regular monitoring, medication may be prescribed to help manage diabetes. This may include oral medications or insulin injections. It is important to work closely with a healthcare provider to determine the most appropriate medication and dosage for your specific needs.
Conclusion
Early symptoms of diabetes should never be ignored as timely detection can significantly impact your health. From unexplained weight loss to frequent urination, recognizing these signs is crucial. Knowing the risk factors, managing lifestyle choices, and understanding treatment options are key to preventing complications. Making healthy changes like diet modifications and regular monitoring can make a substantial difference in managing diabetes. Remember, early intervention is key. Don’t hesitate to seek medical advice if you notice any of these symptoms. Stay informed, stay healthy. Subscribe for more insightful updates on diabetes awareness.
Frequently Asked Questions
Can these symptoms appear suddenly?
Yes, symptoms of diabetes can appear suddenly or develop gradually over time. It is important to be aware of the early signs of diabetes and seek medical attention if you experience any of these symptoms, especially if they are persistent or concerning.
How does diabetes affect daily life?
Diabetes can have a significant impact on daily life. It requires regular monitoring of blood sugar levels, adherence to medication regimens, making dietary and lifestyle changes, and managing the risk of complications. It is important to work closely with a healthcare provider to develop a comprehensive management plan and address any challenges or concerns.
Can making lifestyle changes reverse diabetes?
While lifestyle changes, such as adopting a healthy diet and engaging in regular physical activity, can help manage diabetes and improve blood sugar control, they may not reverse the condition entirely. However, making positive lifestyle changes can significantly reduce the risk of complications and improve overall health and well-being.
What is the difference between Type 1 and Type 2 diabetes?
Type 1 diabetes is an autoimmune disease in which the body’s immune system attacks and destroys insulin-producing cells in the pancreas. Type 2 diabetes, on the other hand, occurs when the body becomes resistant to insulin or doesn’t produce enough insulin. Type 2 diabetes is more common and often associated with lifestyle factors.
Are there any lifestyle changes that can help prevent or manage diabetes?
Yes, adopting a healthy lifestyle can help prevent or manage diabetes. This includes maintaining a healthy weight, engaging in regular physical activity, following a balanced diet, and monitoring blood sugar levels. Managing stress and getting enough sleep are also important factors in diabetes prevention and management.